Help!!! Clueless about Flow Limitations
Re: Help!!! Clueless about Flow Limitations
Jeff, you have earned a million passes on this board----and rarely need to spend them I might add. Wish I could do so well!
- Bright Choice
- Posts: 596
- Joined: Fri Jan 14, 2011 5:17 pm
Re: Help!!! Clueless about Flow Limitations
First, a million thanks to all of you for such thoughtful replies. I understand some of the info and much is over my head - but I have not disappeared and have been watching all of the posts with a great deal of interest.
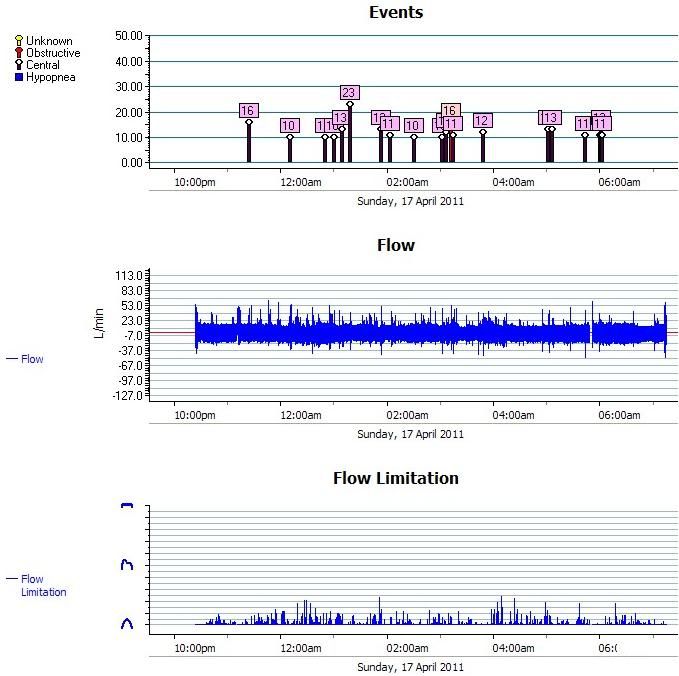
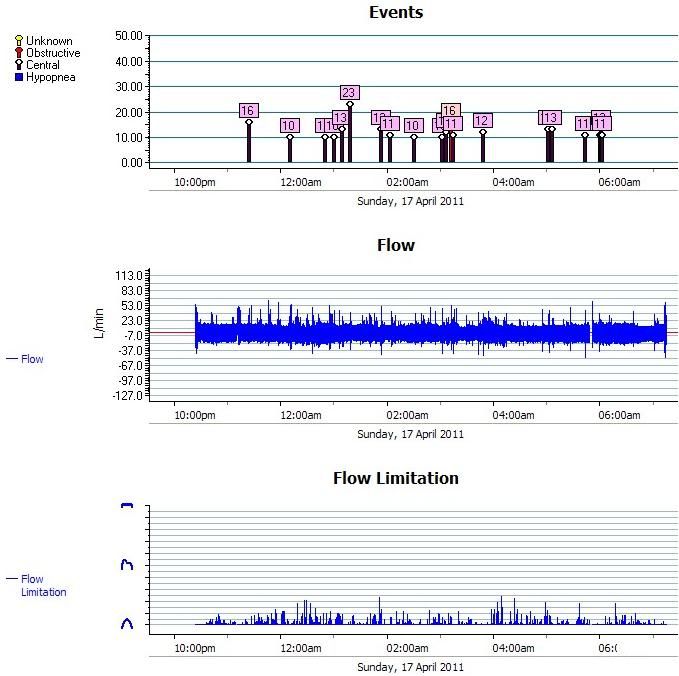
Following is a chart from Rescan showing flow, fl, and event for one night. My initial question stems from how in the world can I "titrate" myself with my autoset when I have no OA, or hypoxic events. It is the flow and fl's that I am curious about - and how I would go about treating them:
Following is a summary of my situation - I tried to be brief but...
I was diagnosed with “mild sleep apnea in the form of upper airway resistance syndrome”. Symptoms included severe insomnia, occasional gasping episodes when awakening, very minimal snoring, eds, fatigue, depression, irritable bowel, postural hypotension, irritability, an easy “startle” reflex and nocturia (4-6 times per night), hypothyroidism. I am 5’4”, 126#.
I had RLS prior to diagnosis, am on Requip but I think cpap has improved RLS. Hope to get off the Requip but will not do that now as I don’t want to “muddy the water”. PLM was present but minimal at psg.
My stats (both at time of PSG and on rescan resports) rarely show obstructions or hypopneas – it is always CA events although I did NOT have a lot of CA’s at PSG.
Diagnosis also included significant insomnia. That disappeared immediately with initiation of cpap and I was off Lunesta within a week – that was a very happy story in itself.
Currently I have daytime fatigue and sleepiness, foggy brain, frequent awakenings, feel “hung over” sans alcohol. I get occasional aerophagia and also have symptoms of upper esophagus reflux (LPR) which I believe have improved since starting Prilosec 2 weeks ago.
Initially, I was told to “try” CPAP at titrated pressure of 5cm to see if it helped. I started monitoring spo2 nightly and when I reported desats to md, he just said to try adjusting the pressure to see if I could get rid of desats. MD said that if CPAP didn't help that my next best option might be to "do nothing at all".
I tried autoset and it seemed to “settle in” around 9 or 10, but no change in desats. The only time I noticed an improvement was when I turned on EPR to 2, but that improvement is inconsistent. I can have 3 to 5 minutes <88%. I had one night where I accidentally slept with mask off for 30 minutes, spo2 desats <88% was 7.7 minutes and one night when I slept at elevation of 9600 ft it was 22 minutes. (I live at 6200 ft). Low is usually in low 80’s. Average for the night 90-92%. I don’t believe I have any daytime desats. I ski 3-4 times a week at altitude up to 12,000 ft with no respiratory problems.
Does UARS correlate with desats? If not, what is causing the desats if I am not having obstructive events or hypopnic events.
I am not sure that I am getting the right xpap therapy. How do I know that the pressure is correct if I have no obstructions or hypopneas to monitor with pressure changes. CA seems to be all over the place, regardless of pressure. Way too confusing to me.
My psg did not qualify me for Medicare so I bought my S9 out of pocket. Medicare will not approve another psg. I am doing a “home” psg this week to see if I can get a high enough AHI to qualify for Medicare, but I have a feeling that AHI will still be low. My doc does not get too excited about filing an appeal under Medicare to get me qualified under UARS diagnosis, nor do I get the sense that he feels he needs to “treat” the UARS. “Your numbers look fine”
I planning on getting a “second opinion” in order to: a) get another sleep study which will be paid by Medicare since it is being done as a “second opinion”, b) get approval under Medicare for UARS and c) hopefully get a diagnosis and therapy that is appropriate for me. It has been suggested that I may be headed for vpap.
Any comments or suggestions would be greatly appreciated! Thanks!!
Following is a chart from Rescan showing flow, fl, and event for one night. My initial question stems from how in the world can I "titrate" myself with my autoset when I have no OA, or hypoxic events. It is the flow and fl's that I am curious about - and how I would go about treating them:
Following is a summary of my situation - I tried to be brief but...
I was diagnosed with “mild sleep apnea in the form of upper airway resistance syndrome”. Symptoms included severe insomnia, occasional gasping episodes when awakening, very minimal snoring, eds, fatigue, depression, irritable bowel, postural hypotension, irritability, an easy “startle” reflex and nocturia (4-6 times per night), hypothyroidism. I am 5’4”, 126#.
I had RLS prior to diagnosis, am on Requip but I think cpap has improved RLS. Hope to get off the Requip but will not do that now as I don’t want to “muddy the water”. PLM was present but minimal at psg.
My stats (both at time of PSG and on rescan resports) rarely show obstructions or hypopneas – it is always CA events although I did NOT have a lot of CA’s at PSG.
Diagnosis also included significant insomnia. That disappeared immediately with initiation of cpap and I was off Lunesta within a week – that was a very happy story in itself.
Currently I have daytime fatigue and sleepiness, foggy brain, frequent awakenings, feel “hung over” sans alcohol. I get occasional aerophagia and also have symptoms of upper esophagus reflux (LPR) which I believe have improved since starting Prilosec 2 weeks ago.
Initially, I was told to “try” CPAP at titrated pressure of 5cm to see if it helped. I started monitoring spo2 nightly and when I reported desats to md, he just said to try adjusting the pressure to see if I could get rid of desats. MD said that if CPAP didn't help that my next best option might be to "do nothing at all".
I tried autoset and it seemed to “settle in” around 9 or 10, but no change in desats. The only time I noticed an improvement was when I turned on EPR to 2, but that improvement is inconsistent. I can have 3 to 5 minutes <88%. I had one night where I accidentally slept with mask off for 30 minutes, spo2 desats <88% was 7.7 minutes and one night when I slept at elevation of 9600 ft it was 22 minutes. (I live at 6200 ft). Low is usually in low 80’s. Average for the night 90-92%. I don’t believe I have any daytime desats. I ski 3-4 times a week at altitude up to 12,000 ft with no respiratory problems.
Does UARS correlate with desats? If not, what is causing the desats if I am not having obstructive events or hypopnic events.
I am not sure that I am getting the right xpap therapy. How do I know that the pressure is correct if I have no obstructions or hypopneas to monitor with pressure changes. CA seems to be all over the place, regardless of pressure. Way too confusing to me.
My psg did not qualify me for Medicare so I bought my S9 out of pocket. Medicare will not approve another psg. I am doing a “home” psg this week to see if I can get a high enough AHI to qualify for Medicare, but I have a feeling that AHI will still be low. My doc does not get too excited about filing an appeal under Medicare to get me qualified under UARS diagnosis, nor do I get the sense that he feels he needs to “treat” the UARS. “Your numbers look fine”
I planning on getting a “second opinion” in order to: a) get another sleep study which will be paid by Medicare since it is being done as a “second opinion”, b) get approval under Medicare for UARS and c) hopefully get a diagnosis and therapy that is appropriate for me. It has been suggested that I may be headed for vpap.
Any comments or suggestions would be greatly appreciated! Thanks!!
_________________
| Mask: Mirage™ FX For Her Nasal CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: S9 VPAP Adapt, CompSA, RLS/PLMD, Insomnia, started 12/30/10 Rescan 3.14 |
- SleepingUgly
- Posts: 4690
- Joined: Sat Nov 28, 2009 9:32 pm
Re: Help!!! Clueless about Flow Limitations
Whenever I see a bunch of central apneas, I know I cannot offer much help. So you never had an official titration? Do you feel like you are waking up a lot? I wonder if those centrals are from waking up. I really must shut up, as I have no idea what I'm talking about.
_________________
| Mask: Swift™ FX For Her Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Rescan 3.10 |
Never put your fate entirely in the hands of someone who cares less about it than you do. --Sleeping Ugly
- Bright Choice
- Posts: 596
- Joined: Fri Jan 14, 2011 5:17 pm
Re: Help!!! Clueless about Flow Limitations
SU you are great!SleepingUgly wrote:Whenever I see a bunch of central apneas, I know I cannot offer much help. So you never had an official titration? Do you feel like you are waking up a lot? I wonder if those centrals are from waking up. I really must shut up, as I have no idea what I'm talking about.
I have had 2 sleep studies in the sleep lab. I can't remember the.numbers off hand but all were pretty low. I'll dig them out to post. Diagnosis "mild sleep apnea with uars". On one of them I think I only had 1 ca. Titration stopped at 5cm because they said that level cleared everything up. Seems weird. I don't awaken as often as those ca's appear. When I look at flows up close, there are some pretty weird configurations that show up prior to my awakening but often nothing is scored as an event.
Thanks!
_________________
| Mask: Mirage™ FX For Her Nasal CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: S9 VPAP Adapt, CompSA, RLS/PLMD, Insomnia, started 12/30/10 Rescan 3.14 |
- SleepingUgly
- Posts: 4690
- Joined: Sat Nov 28, 2009 9:32 pm
Re: Help!!! Clueless about Flow Limitations
They titrated to eliminate RERAs? Or to eliminate FLs, even those unassociated with arousals?Bright Choice wrote:Titration stopped at 5cm because they said that level cleared everything up. Seems weird.
Boy, I wish someone would titrate me to 5cm. I can keep my mouth shut using 4cm, so maybe I could with 5cm (but apparently can't at 6cm)! At my titration, they couldn't get me past 10cm because it got to be early morning, I was waking up too much, and had aerophagia, so they ballparked that I need APAP 11-13. That was before my surgery. According to one surgeon, I should expect a drop of only 1-2 cm post-surgery. According to another, it should minimally half my pressure needs. I'm no math genius, but I think 6 is about half of 11-13, and it isn't cutting it. I'm afraid the other surgeon may have been right. Oh well, maybe I'll work my way up to a pressure that works for me. I hope.
_________________
| Mask: Swift™ FX For Her Nasal Pillow CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: Rescan 3.10 |
Never put your fate entirely in the hands of someone who cares less about it than you do. --Sleeping Ugly
- Bright Choice
- Posts: 596
- Joined: Fri Jan 14, 2011 5:17 pm
Re: Help!!! Clueless about Flow Limitations
The sleep study just says that they titrated for uars and that 5 cm was sufficient. ?? We'll see what happens with further studies.SleepingUgly wrote:They titrated to eliminate RERAs? Or to eliminate FLs, even those unassociated with arousals?Bright Choice wrote:Titration stopped at 5cm because they said that level cleared everything up. Seems weird.
Boy, I wish someone would titrate me to 5cm. I can keep my mouth shut using 4cm, so maybe I could with 5cm (but apparently can't at 6cm)! At my titration, they couldn't get me past 10cm because it got to be early morning, I was waking up too much, and had aerophagia, so they ballparked that I need APAP 11-13. That was before my surgery. According to one surgeon, I should expect a drop of only 1-2 cm post-surgery. According to another, it should minimally half my pressure needs. I'm no math genius, but I think 6 is about half of 11-13, and it isn't cutting it. I'm afraid the other surgeon may have been right. Oh well, maybe I'll work my way up to a pressure that works for me. I hope.
_________________
| Mask: Mirage™ FX For Her Nasal CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: S9 VPAP Adapt, CompSA, RLS/PLMD, Insomnia, started 12/30/10 Rescan 3.14 |
Re: Help!!! Clueless about Flow Limitations
I'll take a stab at a few of your questions/comments, Bright Choice. I hope others can chime in with opinions as well. SU already brought up some excellent points IMO...
I'm under the impression that treatment options for UARS patients entail CPAP, dental appliances, or surgery. While we don't often hear on the message boards that stabilizing UARS-disordered sleep with pharmaceuticals can help, if I had UARS I would probably ask my doctor for experimentation with sleep aids. If I had generalized anxiety symptoms or depression along with those startle reflexes, I would even ask the doctor what he thought about a trial with something like duloxetine (Cymbalta). I think regabalin (Lyrica) might be another nervous system type drug one somatic-disorder/UARS researcher has recently mentioned. I know next to nothing about pharmaceuticals (less than that actually), so please take those comments with a huge grain of salt.Bright Choice wrote: Initially, I was told to “try” CPAP at titrated pressure of 5cm to see if it helped. I started monitoring spo2 nightly and when I reported desats to md, he just said to try adjusting the pressure to see if I could get rid of desats. MD said that if CPAP didn't help that my next best option might be to "do nothing at all".
Sleeping with supplemental O2, at your moderate elevation, just might be another experiment for you and your doctor. Lacking Medicare coverage for supplemental O2, you could always buy a new or used oxygen concentrator if supplemental O2 actually helped with symptoms.I tried autoset and it seemed to “settle in” around 9 or 10, but no change in desats. The only time I noticed an improvement was when I turned on EPR to 2, but that improvement is inconsistent. I can have 3 to 5 minutes <88%. I had one night where I accidentally slept with mask off for 30 minutes, spo2 desats <88% was 7.7 minutes and one night when I slept at elevation of 9600 ft it was 22 minutes. (I live at 6200 ft). Low is usually in low 80’s. Average for the night 90-92%. I don’t believe I have any daytime desats. I ski 3-4 times a week at altitude up to 12,000 ft with no respiratory problems.
If we're talking about Dr. Guilleminault's phenotype, then hyperactive UARS and desats do not go together. However, there are other doctors who do not view UARS and OSA as being mutually exclusive. And I don't think any sleep doctors view RERAs and OSA as being mutually exclusive. But other conditions, besides UARS and OSA, can cause desats.Does UARS correlate with desats? If not, what is causing the desats if I am not having obstructive events or hypopnic events.
Unfortunately the CA part is best understood in light of full PSG data. Those central apneas might be post-arousal, for instance. And the arousals leading to those CAs might be in response to RERAs or PLMs as disruptive stimuli during sleep.I am not sure that I am getting the right xpap therapy. How do I know that the pressure is correct if I have no obstructions or hypopneas to monitor with pressure changes. CA seems to be all over the place, regardless of pressure. Way too confusing to me.
Apnea and hypopnea numbers always look fine for UARS patients according to Dr. Guilleminault's school of thought. Accordingly, the more relevant UARS benchmarks have to do with arousal rate, sleep architecture, and especially daytime symptomology.My psg did not qualify me for Medicare so I bought my S9 out of pocket. Medicare will not approve another psg. I am doing a “home” psg this week to see if I can get a high enough AHI to qualify for Medicare, but I have a feeling that AHI will still be low. My doc does not get too excited about filing an appeal under Medicare to get me qualified under UARS diagnosis, nor do I get the sense that he feels he needs to “treat” the UARS. “Your numbers look fine”
Dr. Krakow, for instance, would treat your flow limitations by raising VPAP's IPAP pressure high enough to round out all your inspiratory flow curves----and by additionally dropping EPAP low enough to round your expiratory curves. That can sometimes make for a large gap between the machine's inhale pressure and exhale pressure. I think that particular UARS treatment approach is also experimental. Good luck!!I planning on getting a “second opinion” in order to: a) get another sleep study which will be paid by Medicare since it is being done as a “second opinion”, b) get approval under Medicare for UARS and c) hopefully get a diagnosis and therapy that is appropriate for me. It has been suggested that I may be headed for vpap.
- Bright Choice
- Posts: 596
- Joined: Fri Jan 14, 2011 5:17 pm
Re: Help!!! Clueless about Flow Limitations
Good comments. I guess I am currently of the thought that if I could some good restorative sleep and the proper xpap therapy that my nervous system would calm down. I’ll keep the rx suggestions in my “back pocket”.-SWS wrote:I'll take a stab at a few of your questions/comments, Bright Choice. I hope others can chime in with opinions as well. SU already brought up some excellent points IMO...
I'm under the impression that treatment options for UARS patients entail CPAP, dental appliances, or surgery. While we don't often hear on the message boards that stabilizing UARS-disordered sleep with pharmaceuticals can help, if I had UARS I would probably ask my doctor for experimentation with sleep aids. If I had generalized anxiety symptoms or depression along with those startle reflexes, I would even ask the doctor what he thought about a trial with something like duloxetine (Cymbalta). I think regabalin (Lyrica) might be another nervous system type drug one somatic-disorder/UARS researcher has recently mentioned. I know next to nothing about pharmaceuticals (less than that actually), so please take those comments with a huge grain of salt.
Actually, I do qualify for supplemental O2 under Medicare, just not for xpap. I tried O2 pre-cpap and it did not make me feel better. Have not tried it with cpap.-SWS wrote:Sleeping with supplemental O2, at your moderate elevation, just might be another experiment for you and your doctor. Lacking Medicare coverage for supplemental O2, you could always buy a new or used oxygen concentrator if supplemental O2 actually helped with symptoms.
I just did 2 nights of home sleep study (without cpap) to see if I can qualify for Medicare.
The first night I did at my home elevation (6200 ft). Miserable night. Had to take Lunesta in order to sleep (I have a big problem with sleep initiation).
First part of the night I was able to sleep on my back and I was aware of a lot of “snorting” myself awake. Then the RLS/PLMD moved in full force. On cpap and with Requip the RLS has been very quiet. Even thinking of trying to go off of it, but I want to get other things squared away first.
In addition to the home machine, I did wear my own oximeter. I had 23 minutes of spo2 desats <88% with a low of 72. It has been running 0-2 minutes on average with cpap.
I spend some time at elevation of 9000 ft so doc wanted a second study done there. Used Lunesta also but just did not sleep well. Spo2 desats <88% was 96 minutes with a low of 72! Hmm...
-SWS wrote:
Dr. Krakow, for instance, would treat your flow limitations by raising VPAP's IPAP pressure high enough to round out
Good comments. I guess I am currently of the thought that if I could some good restorative sleep and the proper xpap therapy that my nervous system would calm down. I’ll keep the rx suggestions in my “back pocket”.
all your inspiratory flow curves----and by additionally dropping EPAP low enough to round your expiratory curves. That can sometimes make for a large gap between the machine's inhale pressure and exhale pressure. I think that particular UARS treatment approach is also experimental. Good luck!!
I am off to “vpap camp” in Albuquerque the first week in May for a "second opinion" and what looks like some “experimentation”. I’m game. If I’m not happy with that route I still have my apap here which isn’t perfect, but I wouldn’t want to live without it. It has really made a huge change in my ability to sleep. (but not so much in my feeling “rested”.)
Thanks for your input SWS!!
_________________
| Mask: Mirage™ FX For Her Nasal CPAP Mask with Headgear |
| Humidifier: S9™ Series H5i™ Heated Humidifier with Climate Control |
| Additional Comments: S9 VPAP Adapt, CompSA, RLS/PLMD, Insomnia, started 12/30/10 Rescan 3.14 |
Re: Help!!! Clueless about Flow Limitations
SWS, could you clarify a few things on the interesting curves you posted:
- re the flow curves, showing some flow limitation and sleep fragmentation effects: I assumed that on your curves, like on my ResScan curves, Inspiration is positive and Expiration is negative relative to average flow. Is that also your convention? some publications reverse the sign convention
- moreover, some papers attribute significance not only to the flow shape, but to the % inspiration time vs. cycle time
- re the flow curves, showing some flow limitation and sleep fragmentation effects: I assumed that on your curves, like on my ResScan curves, Inspiration is positive and Expiration is negative relative to average flow. Is that also your convention? some publications reverse the sign convention
- moreover, some papers attribute significance not only to the flow shape, but to the % inspiration time vs. cycle time
Moderate-severe OSA, ResMed S9 AutoSet EPR + H5i Humidifier, ResMed Masks: trying Swift FX Nasal Pillow, Mirage Nasal, Mirage Quatro or Quattro FX Full Face
ResMed SD card & USB adaptor, ResScan 3.10
ResMed SD card & USB adaptor, ResScan 3.10










